Background:Hemophagocytic lymphohistiocytosis (HLH) is a rare and life-threatening hyperinflammatory syndrome induced by aberrantly activated myeloid and T cells. Primary or familial HLH (pHLH) is a genetic disorder that typically presents in young children. Secondary HLH (sHLH), which can occur at any age but is most common in adults, is triggered by infection, autoimmune disease, malignancy, or other conditions. Without treatment, HLH is universally fatal; even with existing etoposide-based regimens, survival remains low, particularly for malignancy-associated sHLH. There are no approved therapies specifically for sHLH, and most of our understanding of HLH diagnosis comes from studies of pHLH.
The aim of this study is to assemble historical cohorts of sHLH patients from two, large US medical systems to better understand and refine the sHLH clinical definition, characterize demographic, clinical, and treatment characteristics, and compare survival and healthcare resource utilization (HRU) of the cohorts to matched comparison groups. Preliminary findings on the identification of sHLH patients at one US site were previously described [Broome et al., Blood (2022) 140 (Supplement 1): 5490-5491]. Data on sHLH patient identification at both sites are presented here.
Methods: Two Electronic Medical Record (EMR) systems were queried to identify potential patients (site 1: 2009-May 2022 with no age restrictions and site 2: 2006-2022 patients >18 years of age). Three methods were developed for patient identification. Method 1 identified patients with any mention of an HLH-related ICD code (ICD-9 288.4; ICD-10 D76.1, D76.2, D76.3). Method 2 identified patients with combinations of an elevated ferritin value (1,000-10,000 ng/mL or >10,000 ng/mL) or a sCD25 test (predictive markers of malignancy-associated sHLH from the Optimized HLH Inflammatory [OHI] index). Method 3 identified patients with etoposide and dexamethasone treatment, removing patients receiving this treatment as part of a chemotherapy regimen. Full chart review of some cohorts was not logistically feasible because of their size (no ferritin >1,000 AND any sCD25 test, ferritin >10,000 AND no sCD25 test, and etoposide and dexamethasone treatment); in these instances, patient records were screened for a mention of HLH or MAS. At each site, one clinician reviewed all charts, and a second clinician reviewed a random sample. HLH diagnosis was assigned based on expert judgement, and all diagnostic conflicts were resolved between the two clinicians. Clinical and diagnostic data on sHLH patients were pulled from the EMR by the reviewing clinician.
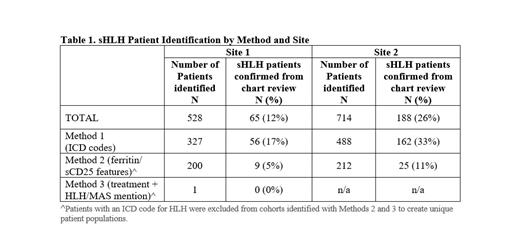
Results: 528 patients were identified at site 1 via the three methods and their charts were reviewed confirming 65 patients with sHLH. Likewise, among 714 charts reviewed at site 2, 188 patients were confirmed with sHLH. Among all patients with an ICD code (Method 1), 17% (56/327) were determined to have sHLH at site 1 and 33% (162/488) at site 2. Among patients reviewed with ferritin/sCD25 features (Method 2), 4% (9/200) were determined to have sHLH at site 1 and 11% (25/212) at site 2. Among patients reviewed with Method 3, 0% (0/1) were determined to have sHLH at site 1, and site 2 data were not available. (See Table 1) Additional analyses on clinical and treatment characteristics of the sHLH cohorts and survival/HRU comparisons will be presented.
Conclusions: Since HLH is a rare, heterogeneous, and complex disease to diagnose and treat, HLH-related ICD codes may not accurately and sufficiently capture the spectrum of HLH patients in EMRs.Clinical indicators of disease were essential for identifying additional patients with this rare disorder. The general consistency of the findings between the two study sites supports the application of this patient identification algorithm across diverse medical centers.
Disclosures
Broome:Argenx; Incyte; Rigel; Sanofi; Star Therapeutics: Research Funding; Alexion; Dianthus: Consultancy. Lai:Electra Therapeutics: Current Employment. Dong:Electra Therapeutics: Current Employment. Fryzek:Electra Therapeutics: Consultancy. Mitchell:Electra Therapeutics: Consultancy. Bylsma:Electra Therapeutics: Consultancy. Daver:Glycomimetics: Research Funding; Amgen: Consultancy, Research Funding; Celgene: Consultancy; Novartis: Consultancy; Jazz: Consultancy; Astellas: Consultancy, Research Funding; Syndax: Consultancy; AROG: Consultancy; Shattuck Labs: Consultancy; Hanmi: Research Funding; ImmunoGen: Consultancy, Research Funding; Daiichi Sankyo: Consultancy, Research Funding; Bristol-Myers Squibb: Consultancy, Research Funding; AbbVie: Consultancy, Research Funding; Genentech: Consultancy, Research Funding; Pfizer: Consultancy, Research Funding; Servier: Consultancy, Research Funding; Agios: Consultancy; Gilead: Consultancy, Research Funding; Trovagene: Research Funding; FATE: Research Funding; Kite, a Gilead company: Consultancy, Research Funding; Novimmune: Research Funding; Trillium: Consultancy, Research Funding; Kronos Bio: Research Funding. Allen:Sobi, Inc: Consultancy.